By Annie Gilbertson and Ben Tanen
February 8, 2024 at 6:00 a.m. EST
Despite being more likely to die of liver disease, Native Americans are far less likely to make the transplant list than Whites

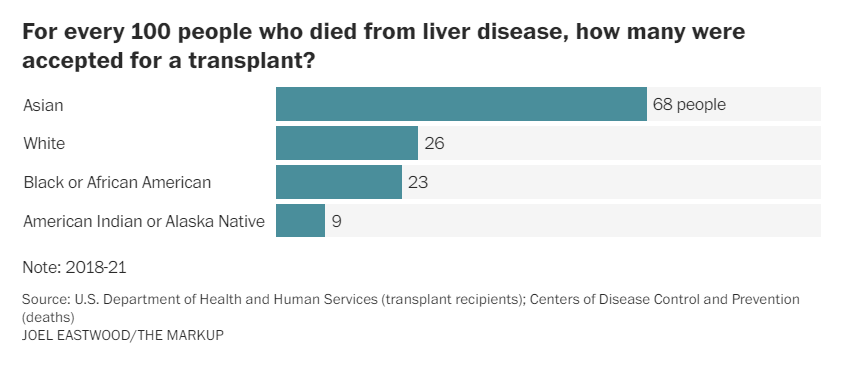
Native Americansare far less likely than other racial groups to gain a spot on the national liver transplant list, despite having the highest rate of death from liver disease, according to an analysis of four years of transplant data by the Markup and The Washington Post.
Compared to their total number of deaths from liver disease, White people gain a spot on the transplant list almost three times more often than Native Americans, the data shows. Had transplant rates been equal, nearly 1,000 additional Native people would have received liver transplants between 2018 and 2021.
Native Americans who do win a spot on the list advance to surgery at about the same rate as White people, showing that front-end access is a primary driver of disparity. Among other racial groups, the liver transplant acceptance rate for Black people is slightly lower than for White patients nationally, while Asian Americans have the highest rate of acceptance to the transplant wait list by far.
These findings come as mortality from liver disease is climbing across the nation, hitting nearly 57,000 deaths in 2021, according to the Centers for Disease Control and Prevention. Liver disease is commonly caused by obesity, hepatitis C and alcoholism. Researchers have attributed the rise in mortality to increased heavy drinking during the coronavirus pandemic, especially among young people.
Data shows poor access to inpatient treatment for alcoholism for tribes across the country. The only cure for end-stage liver disease is a transplant. And getting on the list typically involves referral by a doctor, which can be hard for those with limited resources to access.
U.S. liver disease deaths nearly doubled in two decades
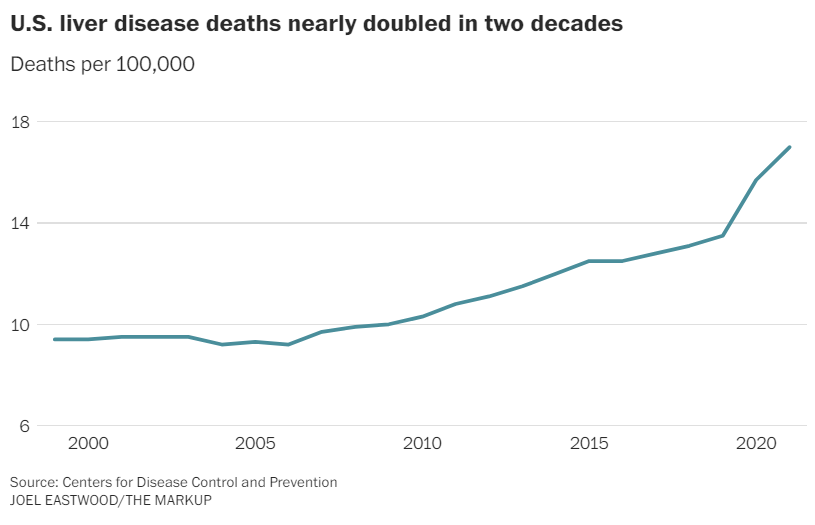
Source: Centers for Disease Control and Prevention
JOEL EASTWOOD/THE MARKUP
Architects of the U.S. transplant system have wrestled with how to equitably distribute the scarce resources since the program’s inception 40 years ago, concerned that organs would flow to the privileged. Yet decades later, inequities persist.
Liver disease deaths have long been an epidemic in Indian Country, where Native Americans are four times more likely to die of liver disease than non-Hispanic White people, according to the U.S. Department of Health and Human Services. It is the second leading cause of death among Indigenous men ages 35 to 44.
Lee Yaiva said every time he went home to the Hopi Reservation in northeastern Arizona, he found that alcoholism had claimed another victim. In July 2022, it was a brother, then in his early 30s. A month later, a second brother died, at 29.
Yaiva said both brothers were aware their drinking had taken a toll on their livers. The family declined an autopsy in the first death. In the second, doctors confirmed that the brother’s liver had shut down. While cleaning out his house, Yaiva discovered dozens of empty bottles of cough syrup, one of the only sources of alcohol on a reservation where it’s not sold.
Living on a rural reservation without cars of their own, the brothers found it difficult to get to the local Indian Health Service (IHS) clinic, the only place where Yaiva said his brothers received medical care. Getting to a transplant center in Phoenix four hours away was unthinkable. He said his brothers never considered a transplant. As far as he knows, the option was not offered.
Yaiva said he believes part of the reason his brothers died untreated was poverty. Transplant professionals agree poverty can be a barrier and add the lack of paid time off and unreliable transportation as other factors.
“They kind of accept” death, Yaiva said. “It has a lot to do with self-worth.”
Loretta Christensen, the IHS’s chief medical officer, said liver disease patients from Indian Country are often diagnosed late, limiting their options. And they may not know a liver transplant is a possibility.
“We need to increase public education,” Christensen said. “We certainly want those who may need a transplant to get that information.”
For this story, The Post and the Markup compared national transplant figures with an indicator of transplant need: therate of liver disease mortality for each racial group, as measured by the CDC. The results: For every 100 Asian people who died of liver disease, approximately 68 patients were accepted for transplant from 2018 to 2021. Among White people, 26 patients were accepted; among Black people, it was 23. (Latinos are assigned to various racial groups in the data and are excluded from this analysis.)
Among Indigenous people, just nine patients were accepted for transplant in that period for every 100 people who died of liver disease.
“The unevenness in access and outcomes is a problem for all of us,” said Jewel Mullen, who has examined disparities in organ transplants and is the associate dean for health equity at the University of Texas at Austin’s medical school.
“They limit our ability to be as healthy as we can be as a society. And I want to believe that at our core [there] is still some fundamental belief in fairness.”
In some parts of the country, racial disparities appeared particularly stark. In D.C. and Arkansas, for example, White people were twice as likely as Black people to be added to the liver transplant list when compared to their rates of death from liver disease.
“It’s not like people saying, ‘Oh, you are Black, you aren’t going to get it,’” said Nikhilesh Mazumder, a gastroenterologist at University of Michigan Health. Mazumder believes it’s more that the history of race in the United States — and its persistent connection to poverty — has “ended up stacking the deck against referral.”
And even small national differences can add up: An estimated 430 additional Black people would have been accepted for liver transplants from 2018 to 2021 had national transplant rates been equal.
A history of problems
In 2022, the National Academies of Sciences, Engineering and Medicine reported that an individual’s chance of being added to the transplant list “varies greatly based on race and ethnicity, gender, geographic location, socioeconomic status (SES), disability status, and immigration status.”
Kenneth Kizer, who chaired the report’s committee and is best known for reshaping the U.S. Department of Veterans Affairs in the 1990s, said “the responsibility lies with HRSA,” the Health Resources and Services Administration, an agency under HHS.
Kizer is not alone in that assessment. When Congress established the Organ Procurement and Transplantation Network in 1984 to oversee the allocation of the nation’s organ supply, lawmakers mandated that a task force convene to make “recommendations for assuring equitable access.”
“We were trying to make sure it would be available for everybody regardless of race or income,” said former Oklahoma senator Don Nickles, a Republican who co-sponsored the legislation. “We wanted the opportunity to be there to save lives.”
For decades, federal law has required the network to increase transplantation among “racial and ethnic minority groups and among populations with limited access to transportation,” but neither the network nor its administrator, the United Network for Organ Sharing, pointed to efforts made to address inequities in access to the liver transplant wait list.
Since 2000, HHS has required the network to collect information about “patients who were inappropriately kept off a waiting list,” but it has never happened.
“If we don’t have that data, we are not going to be able to understand where to intervene,” said Rachel Patzer, an epidemiologist who leads the health research organization the Regenstrief Institute and former chair of the organ network’s data advisory committee. Patzer pushed for 15 years to jump-start the data collection process but said she was stymied by red tape.
Anne Paschke, a spokesperson for the United Network for Organ Sharing, agreed that the data is crucial but said her organization doesn’t have the authority to collect it; HRSA did not dispute that it is holding up data collection and did not answer questions about the more than two-decade delay.
HRSA spokesperson Martin Kramer said in a written statement that the agency is in the midst of the “most significant overhaul of the organ transplantation system in decades,” including plans to improve data collection.
“Letting a lot of young people die”
Experts say data about who is denied transplants could shine a spotlight on inequities at transplant centers.
Because organs are in short supply nationally, transplant teams are selective about who is placed on the list. But no federal rules require transplant centers to make their selection criteria public.
Two centers acknowledge that they will not accept patients with alcohol-associated liver disease unless they are six months sober. The rule stems from fear the new liver would be destroyed by continued drinking. But doctors began abandoning this policy more than a decade ago after research showed that carefully selected patients who had not established six months of sobriety before transplant were nonetheless thriving two years after receiving a new liver.
More than a dozen others either did not respond or declined to provide their policies.
“We were letting a lot of young people die who really should have been transplanted,” Russell Rosenblatt, a transplant hepatologist at Weill Cornell Medicine, said of the six-month rule.
Changes in national policy can improve equity. Before 2002, data showed that Black patients were more likely than White patients to die waiting for a liver transplant. Then, transplant centers rolled out a new way of measuring severity of the disease, so sicker patients could be identified and given higher priority. A study published in 2008 in the influential journal JAMA found this new measurement — known as the MELD score, for Model for End-Stage Liver Disease — radically improved outcomes for Black people on the liver transplant list, wiping out their disparities in deaths in the four years examined.
Donna Cryer, who leads the nonprofit Global Liver Institute, said inequity begins long before a transplant becomes necessary. Patients without access to regular primary care may not be screened for liver disease. The disease is often treated by gastroenterologists or hepatologists, who in turn make referrals to transplant centers when a patients’ illness becomes life-threatening.
“We see a lot of patients drop off” at the specialist stage, Cryer said. “The incentives on finding more people are not there.”
Several transplant experts said lack of reliable transportation and living far from a transplant center can also put the surgery out of reach. Patients on the transplant list must be able to get to routine exams and care leading up to their surgery, and they need to be able to get to a hospital at a moment’s notice should an organ match become available. Patients sometimes move to live near their hospital for this reason — if they can afford it.
Devastation on reservations
In August, Yaiva, the Hopi citizen, was shattered to learn that a third brother had been found dead a week before his 38th birthday.
Though the family again declined an autopsy, Yaiva said, he again suspected years of alcoholism had taken their toll. Near the end, yellowed skin and a bloated body put the often silent, slow-moving disease on sickly display.
“I feel bad for my mom,” he said. “It’s a constant tragedy.”
Yaiva won his own battle with alcoholism a decade ago and went on to become CEO of Scottsdale Recovery Center, which offers culturally informed inpatient programs for Native American clients.
While the Affordable Care Act now requires insurance to cover addiction treatment, Yaiva said many Native Americansstruggle to pay for sober housing and other care to support their sobriety. One in four Indigenous Americans lives in poverty, according to census data, the highest of any racial group.
Citizens of recognized tribes have a right to free health care under federal law following century-old treaties. Still, the IHS fails to provide services needed at many stages of liver disease and addiction treatment, its data shows.
Though the agency serves a population of 2.6 million people with the highest rate of drug- and alcohol-related deaths in the United States, the IHS paid claims for inpatient substance-use treatment for an average of just 18 patients a year from 2018 to 2022.
“The whole country is not getting the addiction treatment that they need broadly, but particularly in Indian Country, there are huge health disparities,” said Monica Skewes, a psychology professor at Montana State University and investigator at the Center for American Indian and Rural Health Equity.
The IHS outsources most addiction treatment to tribal programs, but the quality varies. The Mandan, Hidatsa and Arikara Nation in North Dakota, known as theMHA Nation, is wealthy from oil and gas revenue and has its own inpatient and sober living facilities.
But on the Montana reservation where Skewes does work, she said counselors with little training provide outpatient care. When she began a pilot substance-use treatment program there, community members asked that participants be served full meals instead of snacks, quadrupling the food budget.
“Otherwise, they are literally too hungry to pay attention,” Skewes said.
The IHS has long struggled to pay for services outside its hospitals and clinics. “Many sites were limited to authorizing payment solely for life and limb-threatening emergencies,” IHS spokesperson Nicole Adams said in a written statement.
Adams said recent changes, including the implementation of Medicare-like reimbursement rates, has allowed the agency to stretch its dollars further and provide more services. Lack of addiction treatment is “profound in Indian Country in rural and extreme rural areas,” Adams said, and is a “pressing challenge for the agency.”She declined to comment on whether liver disease care is currently adequate.
IHS officials have repeatedly asked for more federal funding, arguing that it is forced to defer tens of thousands of requests from patients annually for everything from eyeglasses to treatment for sexually transmitted diseases. IHSdata show the agency deferred nearly 113,000 patient requests to see specialists from 2018 to 2022, including 6,196 requests to see gastroenterologists, who treat liver disease and make referrals to transplant centers.
Hepatologists also treat liver disease, but deferrals for that specialty are not broken out in IHS records. However, agency data shows it paid claims for an average of just 226 patients a year to see hepatologists. Rates were similar for gastroenterologists.
IHS patients may sign up for Medicaid, Medicare or seek insurance on Affordable Care Act marketplaces, something IHS staff members routinely recommend. When a patient has access to other coverage, the IHS becomes the payer of last resort.
Claim data shows the agency chipped in very little to the cost of liver transplantation, averaging $11,200 per patient. That is about 2 percent of the $650,000 billed for the average procedure, according to the actuarial and consulting firm Milliman. With medication, recovery and other costs, the price can soar to nearly $900,000.
From 2018 to 2022, the agency kicked in funding for just six liver transplants. During the same period, it deferred 105 requests for transplants of allorgan types.
Adams, the IHS spokesperson, said some requests that are initially deferred may be approved later.
Scarcity extends beyond the IHS. Large swaths of the country have no liver transplant centers, including the Dakotas, Montana, Wyoming and Idaho, which are home to more than two dozen Native Americanreservations.
Monica Mayer is a representative on the Tribal Business Council for the MHA Nation. As a former IHS physician, she has seen firsthand what happens when liver disease is not treated in its early stages. Patients show up in emergency rooms well past the point where their lives might have been saved.
“IHS is not doing a good job of taking care of us,” she said.
Mayer eventually rose to become chief medical officer of the IHS Great Plains Area before serving in tribal government. She said better addiction services are essential to stopping a “devastating” loss of life that has left some small tribes facing cultural extinction.
With every preventable death, Mayer said, “we lose the ability to pass on traditions, our way of life, our language.”
Malena Carollo contributed to this report.
Methodology
To conduct this analysis, reporters obtained data through several Freedom of Information Act requests to the Health Resources and Services Administration, a branch of the U.S. Department of Health and Human Services, and the Indian Health Service.
The response from the HRSA included several anonymized data sets through March 2022 on liver transplants, the donors who provided livers, the candidates waiting for potential transplants, and the hospitals performing liver recoveries and transplants. The IHS provided reports about the number of paid claims for tribal citizens as well as unmet requests. Reporters also used data from the Centers for Disease Control and Prevention on the number of deaths from liver disease and cirrhosis that occurred in each state as an indicator of the need for liver transplants, as all candidates on the liver transplant wait list have end-stage liver disease.
The chief methodological decisions reporters relied on for the analysis included limiting the HRSA data only to adult candidates and transplant recipients; removing candidates needing non-liver transplants, and choosing to focus on transplants, wait list candidates, and deaths between 2018 and 2021.
Using this data, reporters analyzed:
- The ratio of people who die of liver disease vs. those who are added to the liver transplant wait list, compared by racial group.
- The number of claims that the Indian Health Services paid for services related to liver disease care.
- The number of services requested for liver-disease-related care that were deferred by the Indian Health Service.
For a more detailed methodology, including links to the analysis scripts, see the Markup’s full methodology here.
About this story
This report is a joint investigation by The Washington Post and the Markup, a nonprofit newsroom that challenges technology to serve the public good.
Annie Gilbertson is a freelance investigative reporter based in Berkeley, Calif., who writes about criminal justice, technology and education. Ben Tanen is a freelance and data visualization journalist who has worked on stories about unfair practices in the mortgage industry and e-commerce. Malena Carollo is an investigative reporter for the Markup who writes stories that expose broken systems and wrongdoing.
Source:https://www.washingtonpost.com/business/2024/02/08/death-sentence-native-americans-have-least-access-liver-transplant-system/
